Hemocytometer History
The hemocytometer persists as the gold standard for laboratory cell counting. First utilized in 18th century France as a means to analyze patient blood samples, the hemocytometer has gone through a series of major developments over the past hundreds of years, creating a modern instrument that is more accurate and easier to use than its predecessors. The hemocytometer remains an integral part of all cell-based research, and yet sources of error inherent in its design and utilization persist. Let’s take a look at those sources of error and discuss how automation can be employed to eliminate many of these potential pitfalls.
Sources of Hemocytometer Errors
- Human error (mixing, handling, dilution, miscalculation, and procedural errors made by humans)
- Need for multiple cell sample counts to ensure statistical accuracy
- Need for uniform distribution of cells
- Instrumentation and material variation (grids, depth, coverslips, type of buffer, and pipettes)
Resolving Issues of the Hemocytometer
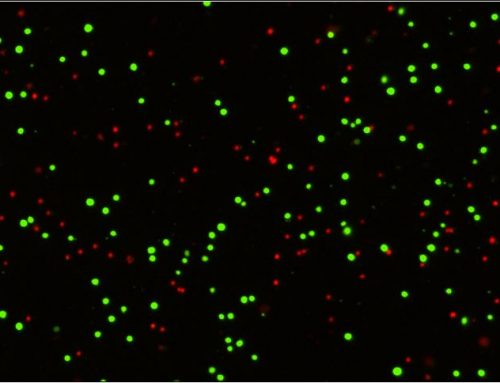
With the development of computers, automation software, optics, fluorescent dyes, and precision manufacturing techniques and modern technologies such as fluorescent microscopy, flow cytometry, and image cytometry, automation has resolved many of the pitfalls associated with the hemocytometer.
Automation resolves:
Human error
In order to resolve this issue, automation and robotics can replace manual liquid handling and counting operations.
Sampling errors
The more fields and cells counted, the lower the random error, but the more time required. By utilizing automated flow or imaging cytometers, thousands to millions of cells can be analyzed in a shorter amount of time, thus increasing efficiency and minimizing the random statistical error in the analysis.
Pipetting and dilution errors
These depend on the technical expertise of the operator. By employing automated pipettes or liquid handling systems, this error can be minimized.26
Material errors
Chamber error occurs due to variation between the different brands of hemocytometer, as well as variation within the same product line. This can also be resolved by using automated cytometers to increase sampling and minimize random error.
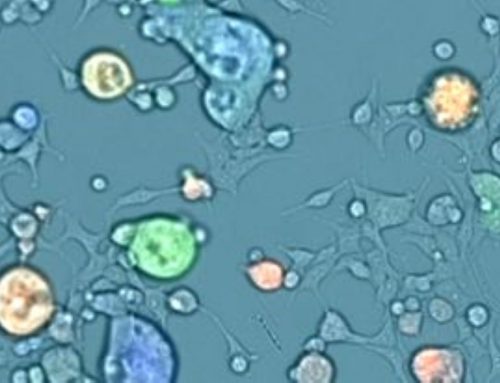
Non-uniform cell distribution
– If a hemocytometer is not cleaned properly, or the coverslip not positioned correctly, variations are generated. These can be eliminated by cytometers that do not utilize chambers such as a flow cytometer. Cell samples that are inherently clumpy will still be difficult for automation. However, by using image cytometers, clumpy cells can be declustered using image analysis algorithms, which can improve the accuracy of cell counting.
Throw out my hemocytometer?
The hemocytometer has been an essential tool in the field of biomedical research for hundreds of years, and it took many iterations to develop the device that researchers use today, yet it remains subject to many unavoidable sources of error. The use of modern automation has largely eliminated many of these sources of error, increasing the accuracy and efficiency of cell counting today.

Leave A Comment